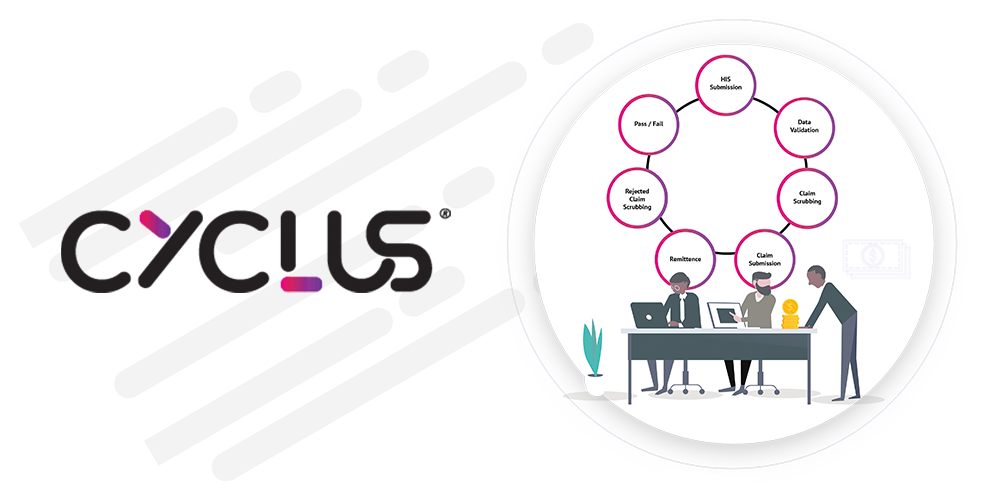
It is a cloud based solution that covers all Revenue Cycle Management processes in order to improve collection payment cycle and reduce claims decline rate.


Its reduce the time between offering a service and receiving payment.
Cyclus is willing to interface with any EHR and accounting system.

Since all financial information are linked to patient record, cyclus allow you to track patient billing and collection easily.
Cyclus enables Health Facilities to perform the RCM duties automatically and save the healthcare providers time and efforts
Cyclus allows you to extract and customized reports upon to your needs.
Cyclus will improve the communication between patients and payers by reminding them of an existing balance and check with insurers when claim is denied
The Eligibilty Module check either directly from payer or from the policy master of the system, for the activation of membership, policy and table of benefit.
The preauthorization modules allows user to insert approvals for procedures/services listed down in the approval request list (for both inpatient & outpatient), so that receptionist or biller can proceed to invoice the listed services.
Create different profile and defined policies, regulations for each type of payers.
This module allows user to define different kind of services in the system with multiple ways of defining prices. Mapping to multiple international coding system like ICD10, ACHI, CPT, CDT, LOINC, Snowmed etc.
Defining procedure prices to insurance claiming facilitation to issuing of invoices happen through this module. The module has numerous functionalities that have been implemented to improve the efficiency as well as accuracy of the transactions.
This module allows end user to list all claims, finds the errors, fix errors and edit healthcare data like: adding diagnosis to make the claim ready for sumissions and upload to payers either by HL7, or API's, XML based, or Excel sheets etc